Hi, Dr Boone,
Thanks so much for accepting questions! I found you through Lani Simpson's Master Class.
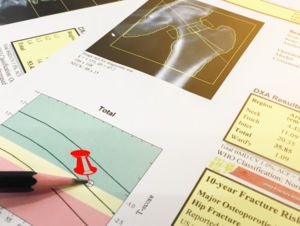
My PTH has been between 24 and 44, calcium between 9.1 and 9.5, phosphorus between 3.9 and 4.3 and vitamin D between 47 and 64 over the last 4 years (I've been on vitamin D supps for at least 2 decades). I could dig up numbers from the years before, but I don't think there was ever much difference. Reason I'm asking is that I lost 19% of my forearm bone density over the course of those 4 years (11% at spine, and 1.5% at hip).
No gastric bypass, I'm an omnivore, no diarrhea. Kidney function normal. I take only 40mg calcium in the form of bone meal. The reason I take so little is that 2-3 years ago, when I did a 24h urine calcium test while taking 400mg calcium supp a day and DIDN'T stop taking it when doing the test, I was at 301 (whatever the unit is). Then I repeated that test 2 months later, and didn't take any calcium supp, and the result was 205. Both my doctors told me it was unnecessary to take calcium supps in that case. I "compromised" and kept taking 40mg.
I just want to cover my bases by making sure whether or not I'm losing so much bone because of my parathyroid, since this affects any kind of treatment plan.
Hi, thanks for writing in! If you are in Lani's group then you are in good hands.
Parathyroid disease often causes bone loss, and the most severe bone loss in parathyroid disease is often seen in the forearm. That is, when someone with parathyroid disease gets osteoporosis, we often see the worst numbers in the forearm, or radius, as opposed to the femur or lumbar spine. So when someone has...