Thank you for taking time to answer questions.
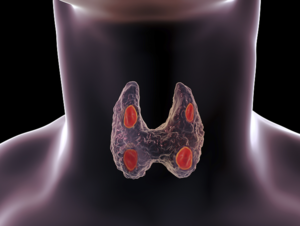
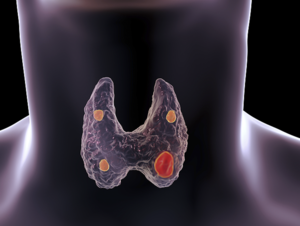
I had 3 1/2 parathyroids removed six months ago. A month after surgery my PTH was 42 pg/ml, Vitamin D 25-OH was 38 ng/ml, but I’m confused what my calcium was as there were two results on the same day. One calcium level (in the metabolic panel) was 9.7 mg/dl and the other one that was listed with the PTH was 10.2 mg/dl. This confused me, but I felt better than I had in years so I wasn’t worried. However, it didn’t last long. The bone pain, fatigue and brain fog ( to name a few) returned and consistently have gotten worse.
I have been taking calcium with vitamin D and magnesium as instructed after surgery. About 3 weeks ago I stopped taking it because the bone pain has gotten worse and I feared my calcium was high again. I am right back to feeling like I did pre surgery. I’m very disappointed and discouraged.
My most recent lab results show that my calcium is 10.2 mg/dl. My vitamin D is 23 ng/ml and PTH is 17 pg/ml. I am 53 years old.
What would cause my calcium to still be high and my other numbers to be so low? I’m so confused.
I should probably mention I have an identical twin sister who has had a parathyroidectomy as well and still doesn’t feel well either, but she had a one sided surgery.
Thank you for your time and I look forward to your response.
Thanks for writing. Your case is complex, and there are a few separate issues to unpack here.
First, let's look at your most recent labs. Your calcium is 10.2 mg/dl, which is high for your age. Your PTH level is 17 pg/ml, which is low, in the suppressed range. This is a good sign, indicating that your remaining parathyroid tissue is responding appropriately to the high calcium. We want the ...











.png)
.png)
.png)











.png)
